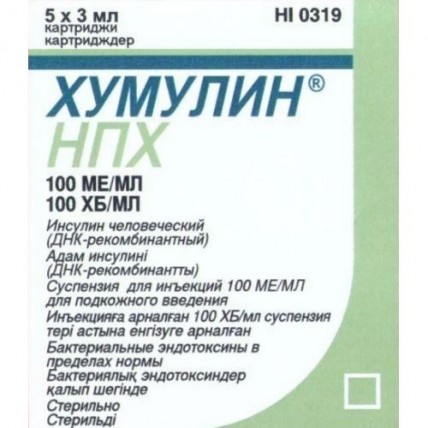
Humulin® NPH 100IU/ml 5x3ml suspension for injection
- $125.00
Out Of Stock
Buy Humulin® NPH 100IU/ml 5 x 3ml suspension for injection
Dosage form
Suspension for subcutaneous administration of white color, which exfoliates, forming a white precipitate and a transparent colorless or almost colorless supernatant liquid; the precipitate is easily resuspended with gentle shaking.
Composition
insulin isophane (human genetically engineered) 100 IU
Excipients: metacresol - 1.6 mg, glycerol - 16 mg, phenol - 0.65 mg, protamine sulfate - 0.348 mg, sodium hydrogen phosphate heptahydrate - 3.78 mg, zinc oxide - q.s. to obtain Zn2 + no more than 0.04 mg, water d / i - up to 1 ml, hydrochloric acid solution 10% - q.s. up to pH 6.9-7.8, sodium hydroxide solution 10% - q.s. to pH 6.9-7.8.
Pharmacodynamics
DNA recombinant human insulin. It is a medium-acting insulin preparation.
The main action of the drug is the regulation of glucose metabolism. In addition, it has an anabolic effect. In muscle and other tissues (with the exception of the brain), insulin causes rapid intracellular transport of glucose and amino acids, accelerates protein anabolism. Insulin promotes the conversion of glucose to glycogen in the liver, inhibits gluconeogenesis, and stimulates the conversion of excess glucose to fat.
Pharmacokinetics
Humulin NPH is a medium-acting insulin preparation.
The onset of action of the drug is 1 hour after administration, the maximum effect is between 2 and 8 hours, the duration of action is 18-20 hours.
Individual differences in insulin activity depend on factors such as dose, choice of injection site, and physical activity of the patient.
Side effects
Side effect associated with the main action of the drug: hypoglycemia.
Severe hypoglycemia can lead to unconsciousness and (in exceptional cases) death.
Allergic reactions: local allergic reactions are possible - hyperemia, swelling or itching at the injection site (usually stop within a period from several days to several weeks); systemic allergic reactions (occur less often, but are more serious) - generalized itching, difficulty breathing, shortness of breath, decreased blood pressure, increased heart rate, increased sweating. Severe cases of systemic allergic reactions can be life threatening.
Others: the likelihood of developing lipodystrophy is minimal.
Special conditions
The transfer of a patient to another type of insulin or to an insulin preparation with a different trade name should be carried out under strict medical supervision. Changes in insulin activity, type (eg, Regular, M3), species (porcine, human insulin, human insulin analog) or production method (DNA recombinant insulin or animal insulin) may necessitate dose adjustment.
The need for dose adjustment may be required as early as the first administration of a human insulin preparation after an animal insulin preparation, or gradually over several weeks or months after transfer.
The need for insulin may decrease with insufficient function of the adrenal glands, pituitary gland or thyroid gland, with renal or hepatic insufficiency.
With some illnesses or with emotional stress, the need for insulin may increase.
Dose adjustments may also be necessary if you increase your physical activity or change your usual diet.
Symptoms-precursors of hypoglycemia during the administration of human insulin in some patients may be less pronounced or differ from those observed during the administration of insulin of animal origin. With the normalization of blood glucose levels, for example, as a result of intensive insulin therapy, all or some of the symptoms, precursors of hypoglycemia, may disappear, and patients should be informed about this.
Symptoms-precursors of hypoglycemia may change or be less pronounced with a prolonged course of diabetes mellitus, diabetic neuropathy, or with the simultaneous use of beta-blockers.
In some cases, local allergic reactions can be caused by reasons not related to the action of the drug, for example, skin irritation with a cleansing agent or improper injections.
In rare cases of development of systemic allergic reactions, immediate treatment is required. Sometimes you may need to change insulin or desensitization.
Influence on the ability to drive vehicles and use mechanisms
During hypoglycemia, the patient's ability to concentrate may deteriorate and the speed of psychomotor reactions may decrease. This can be dangerous in situations in which these abilities are especially needed (driving a car or operating machinery). Patients should be advised to take precautions to avoid hypoglycemia while driving. This is especially important for patients with mild or absent symptoms that predict hypoglycemia or with frequent hypoglycemia. In such cases, the physician should assess the appropriateness of the patient's driving.
Indications
- diabetes mellitus in the presence of indications for insulin therapy;
- newly diagnosed diabetes mellitus;
- pregnancy with type 2 diabetes mellitus (non-insulin dependent).
Contraindications
- hypoglycemia;
- hypersensitivity to insulin or to one of the components of the drug.
Drug interactions
The hypoglycemic effect of Humulin NPH is reduced by oral contraceptives, corticosteroids, thyroid hormone preparations, thiazide diuretics, diazoxide, tricyclic antidepressants.
The hypoglycemic effect of Humulin NPH is enhanced by oral hypoglycemic drugs, salicylates (for example, acetylsalicylic acid), sulfonamides, MAO inhibitors, beta-blockers, ethanol and ethanol-containing drugs.
Beta-blockers, clonidine, reserpine can mask the manifestation of symptoms of hypoglycemia.
Pharmaceutical interactions
The effects of mixing human insulin with animal insulins or human insulin from other manufacturers have not been studied.
Mode of application
Dosage
The dose is set by the doctor individually, depending on the level of glycemia.
The drug should be administered subcutaneously, possibly intramuscularly. IV injection of Humulin NPH is contraindicated!
S / C the drug is injected into the shoulder, thigh, buttocks or abdomen. The injection site must be alternated so that the same site is used no more than about 1 month.
When administered subcutaneously, care must be taken to avoid entering the blood vessel. After injection, do not massage the injection site. Patients should be trained in the correct use of insulin delivery devices.